

Academics
Senior Consultant and Head Clinical and Radiation Oncology HCG cancer Center from 4th April 2016 to till date.
News
ADVANCED CANCER TREATMENT
Towards invasion and conquest of cancer
With cancer cases rocketing in India, a Rs 15,855-crore plan for its early diagnosis and treatment has been included in the 12 th 5 year plan 2012 -2017. This is the largest chunk of India's overall budget for non-communicable diseases (Rs 58,000 crore — a 500% increase from the 11th Plan).
By 2017, India plans to open two national cancer institutions, 20 state cancer institutions along with supporting 100 tertiary cancer centres.
The plan is also to increase district cancer centres from 100 to 640 by end-2017, add 500 additional cancer specialists trained in its management besides training 640 district cancer teams.
Over the next five years, the number of institutes working on India's cancer registry will go up from 27 to 122.
There are about 28 lakh cases of cancer at any given point of time in India with 10 lakh new cases occurring every year. About 7 lakh deaths occur in the country annually due to cancer. .
Cancers account for 14% of the overall NCD mortality in India, and about of 3.3% of the disease burden and about 9% of all deaths. Cancer is a major public health concern in India and has become one of the 10 leading causes of death in the country. The burden of cancer is expected to further increase due to increase in life expectancy, demographic transitions and the effects of tobacco. Around 40 % of cancer cases are due to tobacco use
According to connoisseurs, over 70% of cancer cases in India are diagnosed during the advanced stages of the disease, resulting in poor survival and high case mortality rates. The leading sites of cancer ar e the oral cavity, lungs, oesophagus and stomach among men and cervix, breast and oral cavity among women Cancer of the breast takes the number on e spot in the urban regions
Among men, cancers of the prostate, colon, rectum and liver have shown statistically significant increase in incidence.
The health ministry has allowed every professor of three disciplines radiation oncology, medical oncology and surgical oncology to teach three students as against the existing norm of two. Besides, associate professors across all specialities will be allowed to take on two students under their guidance as against one as per the present norm.
Assistant professors who qualify to be associate professors will also be allowed to take one student under their care. Doctors across 21 states are also getting a one-year crash course in oncology, especially training them on early detection of cancer symptoms and how to deliver chemotherapy.
Cancer is curable if detected early. The results of treatment in stage I and II (early stage) are about 80%. In late stage diseases (stage III and IV), the results are less than 20%. According to the National Programme for Prevention and Control of Cancer announced in June, 2010, 65 tertiary cancer centres (TCCs) that would carry out screening, biopsy and treatment of cancer will be set up in 21 states.
District hospitals are also being strengthened to diagnose and treat patients with chemotherapy. Radiation therapy, however, will be available in 27 existing regional cancer centres, all of which are being upgraded.
The ministry is also giving Rs 1 crore to each district hospital just to provide free chemotherapy to 100 patients per district. The ministry will give Rs 100 crore (estimated cost of chemotherapy per patient per year being Rs 1 lakh) to the 100 shortlisted district hospitals only to provide free chemotherapy.
The 38 new cancer centres will be linked to district hospitals. Auxiliary Nurse Midwives (ANM) are being trained to identify warning signs of cancer while doctors in PHCs and are being trained to diagnose cancer cases early As India moves towards digitalization and E governance access to information and facilities is going to become a lot easier.
According to the Madras Metropolitan Tumour Registry (MMTR), the average annual Age Standardised Rate (ASR; world population reference) of all cancers together was 121.3 per 100,000 among males and 132.8 per 100,000 among females in 2009-2010. The incidence rates of cancer in the childhood (0-14 years) and the geriatric (65+years) age groups were higher among males than females.
The most common forms of cancer among males were that of the lung (ASR: 13.1) followed by stomach (10.9), mouth (7.6) and tongue (6.7); the order among females is breast (35.7), cervix (19.3), ovary (8.0) and stomach (5.9). The trend of cancer incidence between 1982 and 2010 was generally increasing for most of the common cancers, especially tobacco related cancers, among males. Among females, there has been an increasing trend in the incidence of cancers of the breast, ovary, thyroid and lung. The notable decrease has been observed in cancers of the cervix and mouth among women.
The age standardized mortality rate was 34.9 among 100,000 males and 30.2 among 100,000 females. There has been a sharp decline in the frequency of cases registered based on a death certificate only over the years: from 7.5% in 1982-87 to 3.1% in 2006-2010.
We have been warned by WHO that India is the next hub for cancer. Having been practicing Radiation Oncology with a fairly good understanding of the tumour biology based on different age groups, stages for different kinds of cancers and again after a fairly good understanding of the radiobiological aspects which is the basis for getting the best results following irradiation; when it comes to the management of the patient after a histopathologic diagnosis and staging, group discussion is very important. Time and time again I have been stressing on the basis on which a cancer patient needs to be managed. Decision making is no longer a single oncologist’s job. A thorough review of the literature based on results of various clinical trials should be inspected thoroughly. We need to not just look at the available American and the European guidelines but study them seriously and come to a clinical judgement based on our own experiences and practices both academic and clinical, the way it should be. Recent publications hold the key for decision making and desired results. Text books are for reference only, but should be thoroughly read and understood during the period of training
Participation in teaching courses organised by AROI, ESTRO etc. gives us that impetus to train our weapons with high precision to target the target.
Before implementing IG-IMRT, it is very important to describe at least in qualitative terms the inverse treatment planning process and potential issues with all elements involved. List specific contouring requirements for IG- IMRT and, assess the extent to which this requirement is fulfilled in his/her clinical practice. Judge/revise the appropriateness of the dose-volume-constraints used in their clinical practice with respect to the current state of the art. Analyze/ judge treatment plans with regard to applicability, safety and efficacy. Evaluate his/her dosimetry practice with respect to the current standard of practice. Reassess and his/her procedure in producing highly conformal treatment plans. Summarize the overall clinical outcomes and remaining issues with highly conformal techniques across disease entities. Remember to discuss ICRU 50, 62 and 83
Imaging has profoundly improved radiation therapy over the years, particularly considering how 3D data from CT, MRI and PET scans has allowed us to better target gross lesions and increase their understanding of how they are positioned relative to surrounding tissues, Cancers often extend beyond radiographic ally-defined lesions, presenting clinicians with targets that typically can't be identified by imaging.
A real problem occurs, when we design radiation beams and make them too tight when relying on medical imaging. There have been several reports of cancer control rates getting worse when the radiation fields are too tight. The images will only show the gross disease, they don't show the microscopic extensions. So, if you make the radiation fields too tight, you increase the risk of local failure.
I also treat areas that I know from experience, designing radiation fields need to understand where cancers like to spread because that where we should aim our radiation beam. We also need to overcome the impact of motion and geometrical uncertainties on IMRT and IGRT
With adequate funds allocated for the diagnosis and treatment of cancer in the 12th 5 year plan. More Govt centres should be equipped with the state of the art cancer facilities so that the economically weaker section of the society has the access to modern treatment which is the standard of care, and proved to be cost effective. We should be doing the right thing for the right people at the right time. Science and technology should be combined to implement the evidenced based medicine foe a successful outcome It is a great injustice to mankind to deny these facilities to him/her and by treating them with outdated antiquated equipments just because he/she is born poor,
CANCER SCENARIO IN INDIA
In the midst of various diseases, cancer has become a big intimidation to human beings worldwide. Cancer is the second most frequent disease in India accountable for maximum death with about 6 lakh deaths per year. This is due to the reduced accessibility of specialised cancer centres as most of them are centred in state capitals and tier two cities that are involved in prevention, diagnosis and treatment of the disease. All type of cancers have been reported in Indian population including the cancers of breast, cervix, head and neck, rectum, stomach, mouth, lungs, oesophagus, bladder, blood, prostate, liver, skin, etc. The causes of such high incidence rates of these cancers may be both internal akin to genetic, mutations, hormonal, poor immune conditions and external or environmental factors like food habits, industrialization, over growth of population etc.
Anyone living with a history of cancer from the moment of diagnosis through the remainder of life is a cancer survivor. National Cancer Survivors Day is an opportunity to demonstrate that it has an active, productive cancer survivor population and to bring awareness to the challenges they face during and after treatment. Survival rates in India are quite low for most types of cancer, less than half of the advanced countries in many types. More surprising is the fact that survival rates in India are either stagnating, or inching up very slowly, despite India having some of the better treatment facilities. Survival rates are just 19% for stomach cancer compared to 25-30% in most countries, with 58% surviving in South Korea. In India, survival rate for colon cancer is 37% while it is 50-59% in most countries and goes up to 65% in the US. Only 4% of liver cancer patients survive for five years in India compared to 10 to 20% elsewhere. Survival rates have dipped in the case of rectal cancer in India. The main reason for the low survival rates is due the advanced presentation of the disease out of fear and lack of awareness amongst the civic making cure a distant possibility Cancer is curable if detected early. It is very important to impart regular health awareness programmes on a regular basis.
Novel surgical techniques, high precision radiation therapy with pin head accuracy and good psychological care bolstered by anti cancer drugs are all part of the total package we need to offer. For the real future is personalized cancer care: taking into account the individual’s disease and their personal circumstances. However, the extent to which treatment can be tailored to an individual has in the past been limited by crude descriptions of their disease and generic treatment options. Advances in genomics and drug responsiveness are leading to more detailed descriptions of a patient’s cancer and better targeted treatments, which offer significant advantages. Personalized care is the real future for all our patients following group discussion among the Surgical, and Medical and Radiation Oncologists. We need to take into account different views according to the position of each specialist in the cancer care field: from the patient–doctor relationship to the criteria of public health perspectives
Although we have generated more effective therapies in the treatment of cancer we always need to focus with as much attention on how to apply that knowledge to individual patients to realize the goal of personalized care. The best clinical results are achieved for each patient when the patient’s personal values and goals are met. That is really what quality of care is all about: achieving outcomes that matter to patients
Stereotactic Radiosurgery with Cyber Knife for Acoustic Schwannoma
A case report
Dr G Amarnath
Senior Consultant and Head Clinical and Radiation Oncology
HCG Cancer Canter Chennai
Acoustic schwannomas or vestibular schwannomas are benign tumours arising from the Schwann cells of the vestibulocochlear nerve. They are associated with loss of information on chromosome 22. Acoustic Schwannomas either occur on one side as spontaneous mutations or bilaterally as in type 2 neurofibromatosis. Acoustic Schwannomas arise commonly in the internal auditory canal, and later on extend intracranially to the cerebellopontine angle as these tumours cannot erode the bone. Usually occurs in the 5th or 6th decade of life. 95% have ipsilateral hearing loss. A few may have tinnitus, vertigo. Larger tumours may give rise to facial or trigeminal neuropathy.
There is no definite staging system for Acoustic Schwannomas. The following system may be used as a guide for management decisions
Stage I confined to internal auditory canal compressing the vestibulocochlear nerve. First symptoms of unilateral hearing loss and tinnitus usually occur.
Stage II Extension to cerebellopontine angle just away from the cerebellum and the brain stem
Stage III the tumor touches the cerebellum and/or the brainstem, without compression May cause trigeminal and/or facial nerve impaction
Stage IV Cerebellar and brain stem compression symptoms, and/or hydrocephalus The differential diagnosis of CP angle tumours include vestibular schwannomas, meningioma, cholesteatoma, facial or trigeminal schwannomas and rarely primary or metastatic malignant tumours. Treatment options include observation or treatment with Stereotactic Radiosurgery, Stereotactic Fractionated Radiotherapy, and microsurgery. Remedial accomplishment may be calculated by tumour control, as termination of growth or a decrease in tumour size, including preservation of hearing and facial nerve function.
We present a patient diagnosed with Acoustic Schwannoma STAGE 2 who was successfully treated with Stereotactic Radiosurgery using CYBER KNIFE at HCG Enterprises Bengaluru
64 year old gentleman was evaluated by the referring Neurosurgeon for complaints of headache, vertigo and decreased hearing in the left ear of one year duration. CT scan done during March 2018 showed an enhancing extra axial mass measuring 1.5 x 2 cms in the left cerebellopontine angle with extension into and widening the left internal auditory canal. MRI done after 4 days was also corroborative. Findings on radiological imaging were suggestive of Acoustic Schwannoma of the left cerebellopontine angle. In view of comorbidities stereotactic biopsy was not considered. Known case of triple vessel disease for which he underwent CABG on 2011 and stenting of left coronary artery in 2015. He is also a case of diabetes mellitus and hypertension on treatment. Patient was referred to HCG Chennai for further evaluation and management.
On examination he had stable vitals, with normal higher mental functions. Left sensory hearing loss was present. No other cranial nerve abnormality was detected No other motor or sensory deficits. All other systems were normal.
The patient diagnosed to have left CP angle acoustic schwannoma was offered Stereotactic Radiosurgery with Cyberknife at HCG Enterprises Bengaluru with a radical intent to improve local control of the disease. He was not considered for any surgical intervention in view of the comorbidities. Observation was not considered as the lesion was inching closer towards the brain stem. Even though these are slow growing tumours at the rate of 2 mm per year, reports suggest variable and unpredictable growth rates ranging from 2 – 10 mm. The same was discussed with the referral Neurosurgeon.
Planning Procedure
The patient underwent head cast (Orfit) which was utilized for planning CT. The MRI and CT based lesion in the left CP angle along with other critical structures were contoured using MIMVISTA software. The contoured structures were then transferred to the Multiplan system. Planning was evaluated and prescription dose of 25 Gy in 5 fractions was decided. The same was approved
Stereotactic Radio surgery Treatment Procedure
On the days of Radiosurgery treatment, the patient presented to the Cyber knife suite. He was positioned on the Cyber knife treatment table with the performed Orfit that was made and utilised for planning. His position on the table was then registered to the Digital Reconstructive Radiographs. An excellent accuracy registration was confirmed using 6-D Skull Series Tracking Method. Treatment delivery was then commenced. He received total dose of 25 gray in 5 fractions over five uninterrupted days during the first week of April. No undue side effects were encountered during treatment.
The patient is advised tapering doses of steroids for the first three weeks and then pulsed dose every week for two months to counter the side effects of oedema especially in the internal auditory canal
The decision to treat this patent with stage 2 Acoustic Schwannoma with Cyber Knife to terminate the growth that eventually results in decreased tumour size over a period of months versus observation was taken in view of the close proximity of the tumour to the brain stem and its unpredictable growth rate.
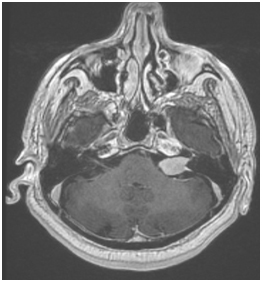
Fig 1 MRI shows Acoustic schwannoma arising from the left Internal auditory canal extending to CP angle
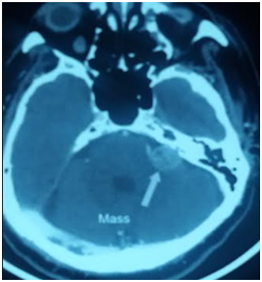
Fig 2 CT scan shows Acoustic schwannoma arising from the left Internal auditory canal extending to CP angle
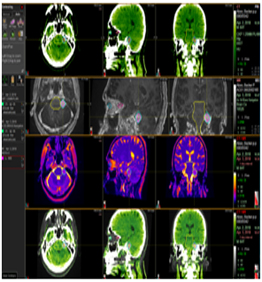
Fig 3 MRI CT point to point fusion for accurate contouring of the target and critical structures
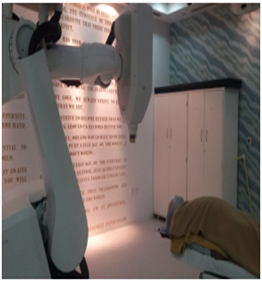
Fig 4 Cyber knife at HCG Bangalore

Fig 5 Target contouring
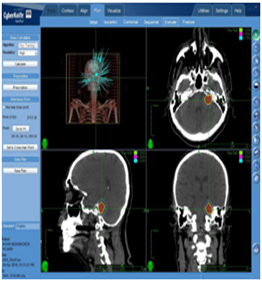
Fig 6 Treatment plan evaluation with different dose levels to the target
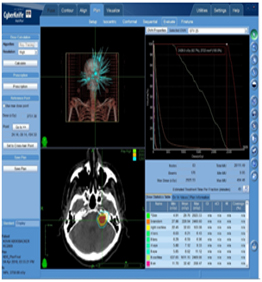
Fig 7 Treatment plan evaluation with different dose levels to the target and surrounding critical structures

Fig 8 6 D skull series tracking method
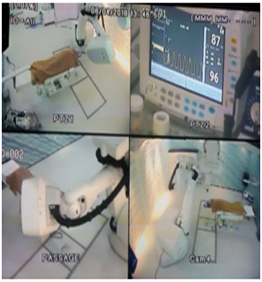
Fig 9 Patient on Stereotactic radio surgery with Cyber knife




